Our therapeutic focus
Schizophrenia
Schizophrenia is a severe mental illness that impacts a person’s thoughts, emotions, and actions. It frequently manifests as a combination of hallucinations, delusions, and disorganized thought and behavior.

Schizophrenia
Imagine a world where your own thoughts feel like a chaotic symphony, a jumble of voices and images that don’t make sense. Imagine believing things that others know are untrue, feeling like you’re being watched or controlled, or struggling to connect with the world around you. This is the reality for people living with schizophrenia.
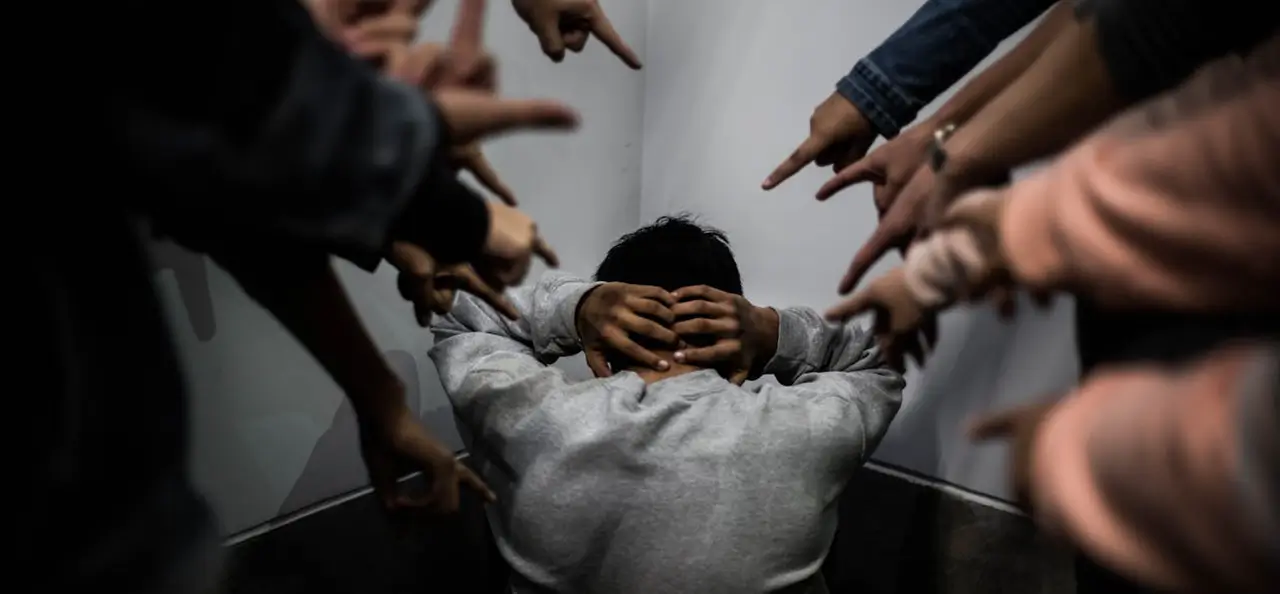
The emotional toll of schizophrenia is immense. The world can feel like a confusing and hostile place, leading to feelings of anxiety, fear, and isolation. It can be difficult to experience joy or pleasure, and some people may struggle with depression. The very core of a person’s sense of self can be affected, leading to feelings of fragmentation and loss. Relationships often suffer, as the illness can make it hard to maintain connections with family and friends. The stigma surrounding mental illness, particularly schizophrenia, can add another layer of pain, leading to feelings of shame and further isolation.
Types of Schizophrenia
The way we talk about different forms of schizophrenia has evolved. While older classifications used terms like “paranoid,” “disorganized,” and “catatonic”, the modern approach recognizes that schizophrenia presents as a range of symptoms with varying degrees of severity.
Nevertheless, it’s important to note that understanding these subtypes, can still be helpful:
1. Paranoid Schizophrenia
Characterized by prominent delusions and auditory hallucinations. Individuals often believe they are being persecuted or plotted against. Despite these intense beliefs, cognitive functioning and affect (emotional expression) may remain relatively intact.
2. Disorganized Schizophrenia
Also known as hebephrenic schizophrenia. It involves disorganized speech and behavior, as well as flat or inappropriate affect. The person may have difficulty with daily activities and personal hygiene.
3. Catatonic Schizophrenia
Marked by disturbances in movement. Individuals may exhibit extremes of behavior, such as remaining immobile in rigid postures for extended periods (catatonic stupor) or excessive, purposeless motor activity (catatonic excitement). They may also display echolalia (repeating others’ words) or echopraxia (mimicking others’ movements).
4. Undifferentiated Schizophrenia
This category was used for individuals who displayed symptoms of schizophrenia but did not fit neatly into the paranoid, disorganized, or catatonic subtypes. It was a more general classification.
5. Residual Schizophrenia
Describes individuals who have a history of schizophrenia but currently exhibit only mild symptoms. Major psychotic symptoms like delusions or hallucinations may have subsided, but some negative symptoms (e.g., lack of motivation, flat affect) or cognitive symptoms may persist.
The modern approach to diagnosing schizophrenia focuses on the severity and range of symptoms overtime, rather than fitting individuals into rigid subtypes. Treatment plans are tailored to the unique needs and symptoms of each person.
Symptoms of Schizophrenia
Imagine your mind as a battleground, where reality and illusion blur, and thoughts become a chaotic maze. This is the reality of schizophrenia, a complex mental illness that distorts perception and impairs clear thinking.
The symptoms of schizophrenia can be incredibly varied and intensely personal, but they can be broadly categorized into three main types:
Positive symptoms:
These are additions to normal experiences, often appearing as:
- Hallucinations: Experiencing things that aren’t real, like hearing voices, seeing things that aren’t there, or feeling sensations that don’t exist. Imagine the terror of hearing voices that command you to do things or constantly criticize you, or the confusion of seeing things that others don’t.
- Delusions: Firmly held beliefs that are not based in reality, like believing you have special powers, that people are trying to harm you, or that your thoughts are being controlled by others. These delusions can be incredibly distressing, leading to fear, paranoia, and a sense of isolation.
- Disorganized thinking and speech: Difficulty expressing thoughts clearly and logically, jumping from one topic to another, or using words in unusual or nonsensical ways. Imagine the frustration of trying to communicate your thoughts and feeling like your words are getting lost in a jumble of confusion.
Negative symptoms:
These are reductions in normal experiences, often leading to:
- Flat affect: Reduced expression of emotions, appearing emotionally flat or unresponsive. Imagine the difficulty of connecting with others when you can’t express your feelings or understand their emotions.
- Alogia: Poverty of speech, speaking very little, or responding in a brief and unelaborated way. Imagine the frustration of wanting to connect with others but finding it hard to find the words to express yourself.
- Avolition: Lack of motivation and interest in activities, feeling apathetic and withdrawn. Imagine the struggle to find the energy and enthusiasm to engage in activities you once enjoyed, feeling like you’re just going through the motions.
Cognitive symptoms:
These affect thinking, memory, and attention, often leading to:
- Problems with attention and concentration: Difficulty focusing, staying on task, or filtering out distractions. Imagine the frustration of trying to read a book or have a conversation but finding your mind constantly wandering.
- Difficulty with working memory: Struggling to hold information in your mind, remember instructions, or complete tasks that require multiple steps. Imagine the challenges of managing daily tasks or learning new things when your mind feels foggy and your memory is unreliable.
- Executive function deficits: Difficulty planning, organizing, and problem-solving, struggling to make decisions, initiate tasks, or manage time effectively. Imagine the difficulties of managing your daily life, feeling overwhelmed by simple tasks and struggling to make even the smallest decisions.
The experience of schizophrenia is unique to each person. Symptoms can fluctuate in intensity and affect individuals in diverse ways. While living with schizophrenia presents significant challenges, effective treatment and support can empower individuals to manage their symptoms and lead meaningful lives.
Causes of Schizophrenia
The exact causes of schizophrenia are intricate and not entirely comprehended, yet research indicates that its development is influenced by a blend of various factors. Let’s delve deeper into these potential causes:
Genetic Factors
- Family History: Individuals with a family history of schizophrenia are at a higher risk. Studies indicate that if a parent or sibling has the disorder, the likelihood of developing it increases.
- Genetic Variations: Certain genetic mutations and variations may predispose individuals to schizophrenia, although no single gene has been identified as the cause.
Brain Chemistry and Structure
- Neurotransmitters: Imbalances in brain chemicals, particularly dopamine and glutamate, are believed to play a significant role in the development of schizophrenia. These neurotransmitters are crucial for communication between brain cells.
- Brain Structure: Some studies have shown that individuals with schizophrenia may have differences in brain structure, such as enlarged ventricles or reduced gray matter.
Environmental Factors
- Prenatal Exposure: Complications during pregnancy, such as infections or malnutrition, may increase the risk of developing schizophrenia later in life.
- Substance Use: Heavy use of substances like marijuana during adolescence has been linked to an increased risk of developing schizophrenia, especially in those with a genetic predisposition.
- Stressful Life Events: Traumatic experiences or significant stressors, particularly during critical developmental periods, can trigger the onset of symptoms in vulnerable individuals.
Psychological Factors
- Cognitive Vulnerabilities: Certain cognitive styles, such as a tendency to misinterpret social cues or have negative thought patterns, may contribute to the risk of developing schizophrenia.
- Social Isolation: A lack of social support and isolation can exacerbate symptoms and may be a contributing factor in the onset of the disorder.
While the exact causes of schizophrenia remain elusive, it is clear that a combination of genetic, biological, environmental, and psychological factors plays a role. Understanding these causes can help in developing effective prevention and treatment strategies.
Supporting Yourself Through Schizophrenia
Managing schizophrenia requires a multifaceted approach encompassing medical care, self-care practices, and community support. This guide provides a comprehensive overview to help you on your journey.
Medical Treatment
1. Follow Your Treatment Plan: Adhere to your medication regimen and attend therapy sessions as prescribed by your healthcare provider. Consistency is key.
2. Regular Check-Ins: Schedule regular appointments with your psychiatrist or mental health professional to monitor your progress and adjust treatment as needed.
Practical Tips
1. Set Goals: Create achievable, realistic goals for yourself. Breaking tasks into smaller steps can make them more manageable.
2. Use Reminders: Utilize calendars, planners, or digital reminders to help you stay organized and remember important tasks and appointments.
3. Seek Support Groups: Join support groups for individuals with schizophrenia. Sharing experiences with others who understand can be very comforting.
Mental Health Support
1. Therapeutic Support: Engage in individual therapy to work through personal challenges and develop coping strategies.
2. Crisis Plan: Have a crisis plan in place that outlines steps to take if your symptoms worsen. Share this plan with a trusted person.
Professional Assistance
1. Case Management: Consider working with a case manager who can help you navigate healthcare systems, access resources, and manage daily activities.
2. Occupational Therapy: An occupational therapist can assist with developing skills for daily living and improving your overall functionality.
Self-Care Strategies
1. Educate Yourself: Learn about schizophrenia and its symptoms. Understanding your condition can help you manage it more effectively.
2. Develop a Routine: Establish a daily routine that includes regular sleep, meals, and activities. Predictability can provide a sense of stability.
3. Stay Connected: Maintain relationships with family and friends. Social support is crucial for emotional well-being.
4. Manage Stress: Practice stress-reducing activities such as yoga, meditation, deep breathing exercises, or mindfulness.
5. Healthy Lifestyle: Incorporate a balanced diet, regular exercise, and adequate sleep into your daily life.
6. Avoid Substances: Stay away from alcohol and recreational drugs, as they can exacerbate symptoms and interfere with medication.
7. Engage in Hobbies: Find activities you enjoy and make time for them. Hobbies can provide a sense of purpose and joy.
Stay Hopeful
Remember, managing schizophrenia is a long-term commitment, but with the right support and strategies, you can lead a fulfilling life. Surround yourself with positive influences, seek help when needed, and be kind to yourself.
Important Reminder
Seeking help is an indication of strength not weakness. Immediate action can save lives; so put safety first and seek help when necessary.
